By Karim Mikhail
The brain. An organ that holds the secret of humanity, whose enigmas continually perplex the brightest researchers. Science has laid bare the secrets of virtually every other organ. Our brain, however, remains the final frontier: a pièce de résistance in human evolution.
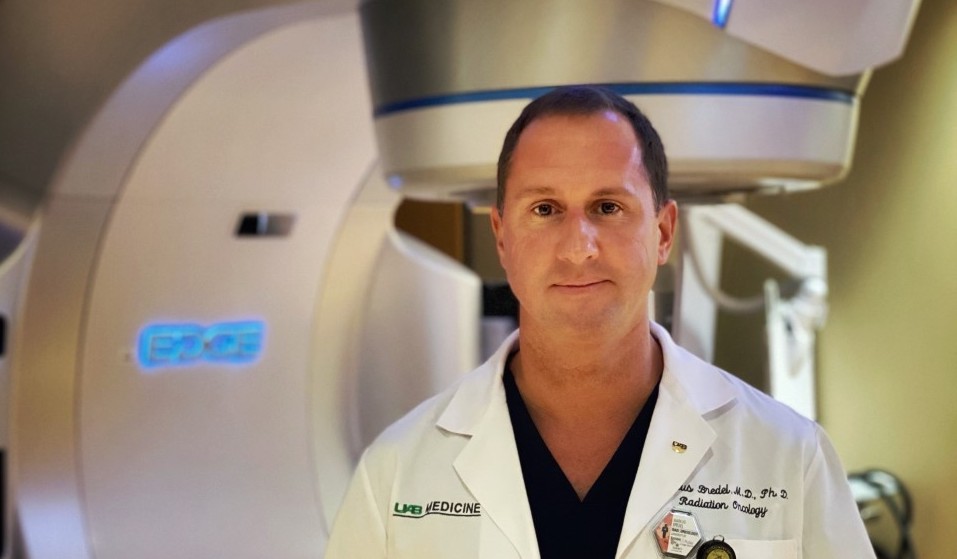
But for all its mysticism, the brain is more accessible than ever before. Technological and medical advancements have enabled scientists and physicians to probe its circuitry, investigating how these networks can go awry when diseased. Dr. Markus Bredel, a central nervous system (CNS) radiation oncologist at the University of Alabama at Birmingham, is one doctor who is leading these advances.
Bredel balances his time between caring for brain cancer patients and heading a basic science research lab. His research focuses on the molecular genetics of primary brain tumors – such as glioblastoma—in search of promising therapeutic avenues for patients. But his story is far from conventional.
“It’s not a straightforward path,” remarks Bredel on his journey to radiation oncology. For him, it began with a passion for studying the brain. Raised in a family of surgeons, he initially sought a career in neurosurgery.
Yet, the field left him yearning for more.
“The more I did neurosurgery, the more I realized that what I really liked within the discipline was the cancer aspect,” adds Bredel. Pivoting to radiation oncology, he is now able to combine his love for neuroscience, cancer care, and cutting-edge medicine.
“Radiation oncology is probably the fastest-moving discipline when it comes to innovation and high-tech,” he says, “and that’s what I really like.”
Nonetheless, CNS oncology is riddled with a plethora of challenges—spanning scientific dimensions of disease to human ones.
Brain cancer is arguably the most devastating diagnosis that a patient can endure. Outcomes are unfavorable, and care is limited to the extension of life rather than a true cure. While immense treatment advances have been made in most cancers, brain cancer trails behind the pack: immune to contemporary treatment. Drawing on his experiences, Bredel attempts to explain why.
“Of course, the biggest issue is the blood-brain barrier,” states Bredel. The blood-brain barrier is a system of blood vessels that tightly regulate what can or cannot enter the brain. This property is in fact advantageous to the brain, ensuring the organ remains free of toxins and functions normally. But in terms of therapy, the blood-brain barrier is a foremost limitation.
“Some chemotherapeutic agents just don’t get into the brain,” states Bredel, “so they can’t be used.” Ongoing efforts focus on novel drug delivery mechanisms that may solve this issue – allowing therapeutics to enter the cryptic domain that lies within.
Alongside these defenses, the growth mechanisms of brain tumors make them more elusive than other cancers.
“Think about colon cancer,” Bredel suggests. “It grows basically as a bulky tumor. The bulkiness of the [cancer] represents 90% of the disease.”
Brain cancer is an entirely different beast. A glioblastoma tumor—the most common brain cancer— “still has a bulky tumor mass, but it’s a small fraction of the actual tumor,” says Bredel. Contrastingly, glioblastoma tumors send out small “tumor fingers” which project along neighboring blood vessels. These fingers can extend their reach to virtually any region in the brain.
“It’s almost like a systemic disease of the brain,” comments Bredel. He adds, “basically any therapy that is locally targeted to the bulk of the tumor will miss much of the tumor.” Consequently, local therapies are rarely curative in brain cancer.
Finally, the extreme heterogeneity of brain tumors complicates treatment. Bredel explains, “one tumor cell is not like another one.” Instead, they might each possess distinct genetic and molecular marks. In other words, therapies that are targeted toward a particular mutation—so-called molecular targeted therapies— “will not hit the whole tumor,” Bredel makes clear.
It might seem feasible, then, to leverage therapies that target a larger area of brain tumors. Enter the double-edged sword of cancer care.
“The broader you target,” explains Bredel, “the more off-target effects you have.”
The body’s molecular pathways are convoluted and intersecting; from an evolutionary perspective, they were never meant to be tampered with. But cancer therapeutics do just this. Ultimately, it falls on cancer physicians to find a middle-ground between killing cancer cells and preserving healthy tissue—a feat that keeps the field progressing forward.
Like much of the world, cancer care has been heavily impacted by the COVID-19 pandemic. From diagnostic complications to technological and philosophical changes in patient care, Bredel has experienced these effects firsthand.
In terms of diagnostics, a PET-CT (positron emission tomography/computed tomography) scan enables radiologists and oncologists to identify areas with higher-than-normal levels of metabolic activity—a clear sign of cancerous cells. Yet, with the onset of COVID-19 and vaccinations, this imaging aspect becomes increasingly complicated.
“You have someone [a cancer patient] with the COVID-19 disease or someone who was vaccinated, and now when you take a PET-CT you see lymph nodes lighting up everywhere else in the body.”
When a cancer patient with COVID-19 or the vaccination receives a PET-CT scan, lymph nodes throughout the body light up, indicating increased activity in those areas.
“Before the pandemic you would think that the activity is progression of the disease,” he says, “but then we found out that this [the activity] was just a reaction of the immune system due to the disease or the vaccine.”
For patients immunocompromised from chemotherapy, encouraging vaccinations became an essential part of Bredel’s duties. “My final question will always be ‘Did you get the booster?’ or ‘Did you get the vaccine?’” he says. “Even if I make a difference for only my patients, we can save lives.”
For Bredel, this human dimension of cancer care is his greatest motivator—and his greatest struggle.
Caring for patients in their last months of life can take a toll on any physician. “On the one hand, all of these patients face potentially life-altering deficits because of these tumors,” says Bredel.
Yet, it’s often these same patients that fill Bredel with hope.
“It is stunning to me how grateful these patients are for the type of therapy they get,” says Bredel. “You have [someone] that’s terminally ill, and now you can change the trajectory of the disease.”
Every day counts in brain cancer care. To extend one’s life by even a few months is an incredible privilege for Bredel. His patients’ formidable strength—from their darkest moments to the triumphant feeling of a cancer-free scan—empower him to persist.
Above all, one case rings true.
“He was a Columbia medical student working in my lab when I was still at Northwestern. He was diagnosed with glioblastoma, and of course, it was a life-shattering experience,” says Bredel. “The striking thing is that he continued working in lab, developing an interest in researching his own tumor. We got a sample of his tumor from the surgery, and we profiled all the 40,000 genes from his tumor.”
The results astonished Bredel and his research team.
“From the genetic profiling, we learned that his tumor was one that might take a less aggressive course. I felt that he might do more favorable.”
And Bredel was exactly right.
“The student finished medical school, completed a pediatrics residency, and got married. He’s almost 14 years out now, without any tumor recurrence.”
It’s cases like these that convey a simple, profound truth of brain cancer care: the path to survival begins with hope.